How Do You Maintain Compliance in Healthcare? (5 Key Steps Explained)

Quick summary
Healthcare compliance isn’t limited to meeting regulations; it’s also about protecting patients, staff, and facilities while avoiding costly penalties. Our guide breaks down five practical steps hospitals can take to maintain compliance. You’ll also see how platforms like Ruya support healthcare systems with real-time floor plans, mobile inspections, and building-level data.
Want to maintain compliance standards in your hospital?
Most compliance failures don’t start with negligence; they start with gaps in systems. A new wing opens before floor plans are updated. Inspection logs live in spreadsheets no one reconciles. Over time, these small disconnects are less visible, leading to a disconnect between what’s on paper and what’s on the ground.
In this Ruya article, we’ll explain how to maintain compliance in healthcare by focusing on process design, data integrity, and real-time coordination.
But first…
Why listen to us?
At Ruya, we partner with leading hospital systems to solve real compliance challenges, from outdated floor plans to disconnected inspections. Built for healthcare, our platform unifies code-based checklists, vendor data, and real-time updates by building. We don’t just talk about compliance; we help hospitals achieve it every day.

What is healthcare compliance?
Healthcare compliance means adhering to the laws, standards, and internal policies that protect patient safety and ensure quality care. It covers everything from data privacy to facility inspections.
Hospitals must prove they meet requirements from regulators like CMS, OSHA, and The Joint Commission.
Compliance also includes managing facility safety, maintaining accurate records, and making sure staff follow procedures. When done right, it creates safer environments for patients and reduces operational risk for healthcare organizations.
Why is healthcare compliance important?
- Patient safety: Compliance ensures safe facilities, proper procedures, and reduced risks of harm or infection.
- Legal protection: Meeting standards shields hospitals from costly fines, lawsuits, and government penalties.
- Audit readiness: Accurate records and inspections make accreditation and regulatory reviews faster and less disruptive.
- Financial stability: Preventing compliance gaps reduces waste, delays, and unexpected expenses.
- Reputation and trust: Consistent compliance builds confidence with patients, staff, and regulators.
How do you maintain compliance in healthcare?
1. Identify and understand regulations and accreditation standards
Healthcare compliance starts with knowing the rules your organization must follow. Regulations don’t just come from one source, but from federal law, state agencies, and accrediting bodies. Each layer adds unique obligations that facility managers must interpret and apply.
For large hospital systems managing multiple assets, this means aligning with CMS standards, OSHA requirements, NFPA codes, and accreditation programs like The Joint Commission. Overlooking even a small clause can put patient safety and reimbursement at risk.
To help your team stay focused, break regulations into actionable categories:
- Clinical requirements: Patient safety, infection control, privacy (HIPAA).
- Facility requirements: Fire safety, life safety codes, and environmental health.
- Operational requirements: Staff training, documentation, and emergency preparedness.
Facilities managers should then map each requirement against current policies, procedures, and assets. The goal isn’t to memorize every line but to identify where your organization is strong and where compliance gaps exist.
2. Standardize inspections and documentation
In large hospital systems, inspections are only as strong as the process behind them. Paper checklists and isolated spreadsheets often create missed items. Standardization eliminates these weak points and brings consistency to every facility.
The most effective teams use digital checklists tied to regulatory codes. This ensures every inspection aligns with external standards and internal policies. It also removes inconsistencies across facilities, so findings can be compared and resolved quickly.
But standardization goes beyond the inspection itself. Documentation must be captured in real time and stored in a structured, accessible format. Disconnected reports create blind spots, while centralized logs help teams respond faster and demonstrate compliance.
When setting up standardized inspections, focus on:
- Consistency: Use the same checklists across every facility.
- Traceability: Store results in one hub that links to floor plans and assets.
- Timeliness: Capture data on-site, not after the fact.
- Accessibility: Make records easy to access for staff, compliance leaders, and auditors.
At Ruya, we strengthen this by providing mobile inspections built on code-based checklists. Facilities staff can log results on-site, flag issues instantly, and keep records accessible across the system. This reduces delays caused by manual uploads and fragmented reporting.

To learn more about documentation, check out our guide on setting up a document control system for hospitals.
3. Update facility data, floor plans, and vendor records
In large hospital networks, keeping drawings, inspection logs, and vendor records synchronized is as critical as the inspections themselves.
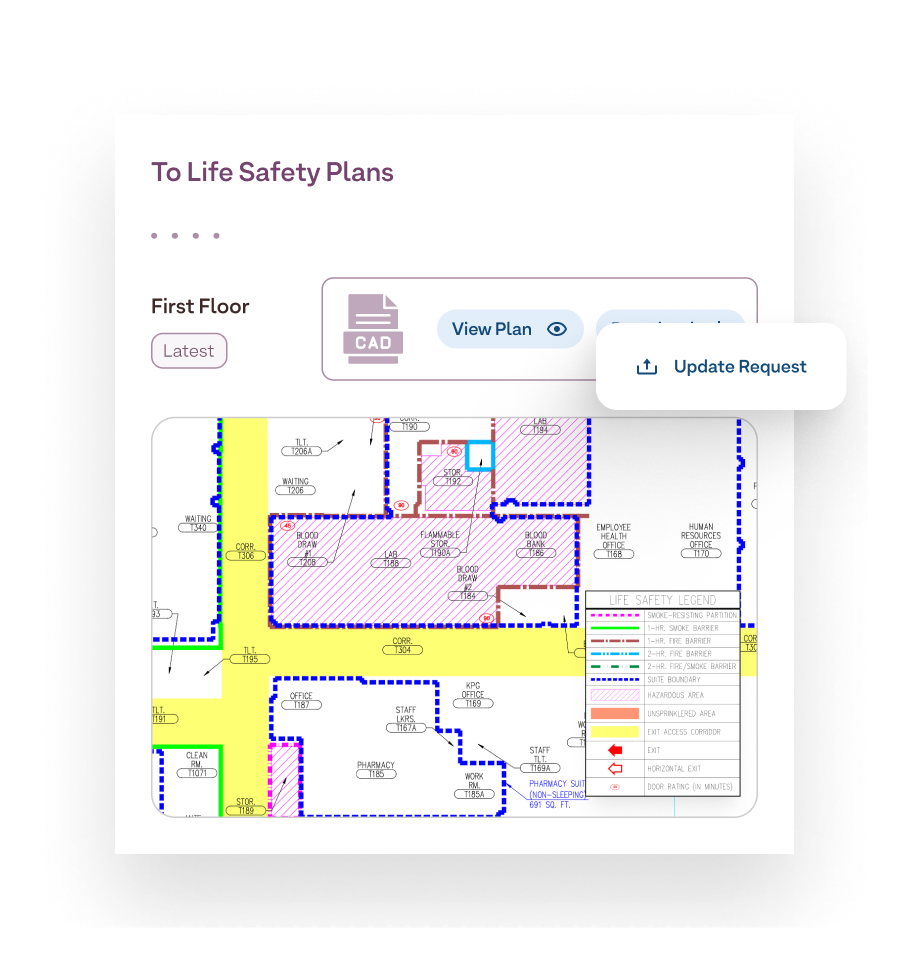
Floor plans are a common weak spot. By the time a new plan circulates, it’s often already outdated, creating risk during safety checks or audits. Hospitals that manage dozens of buildings can’t afford long delays or inconsistent versions.
Vendor and asset records pose similar challenges, too. Teams often rely on email chains or spreadsheets to track who is responsible for specific systems. When those records are scattered across multiple systems, compliance gaps appear.
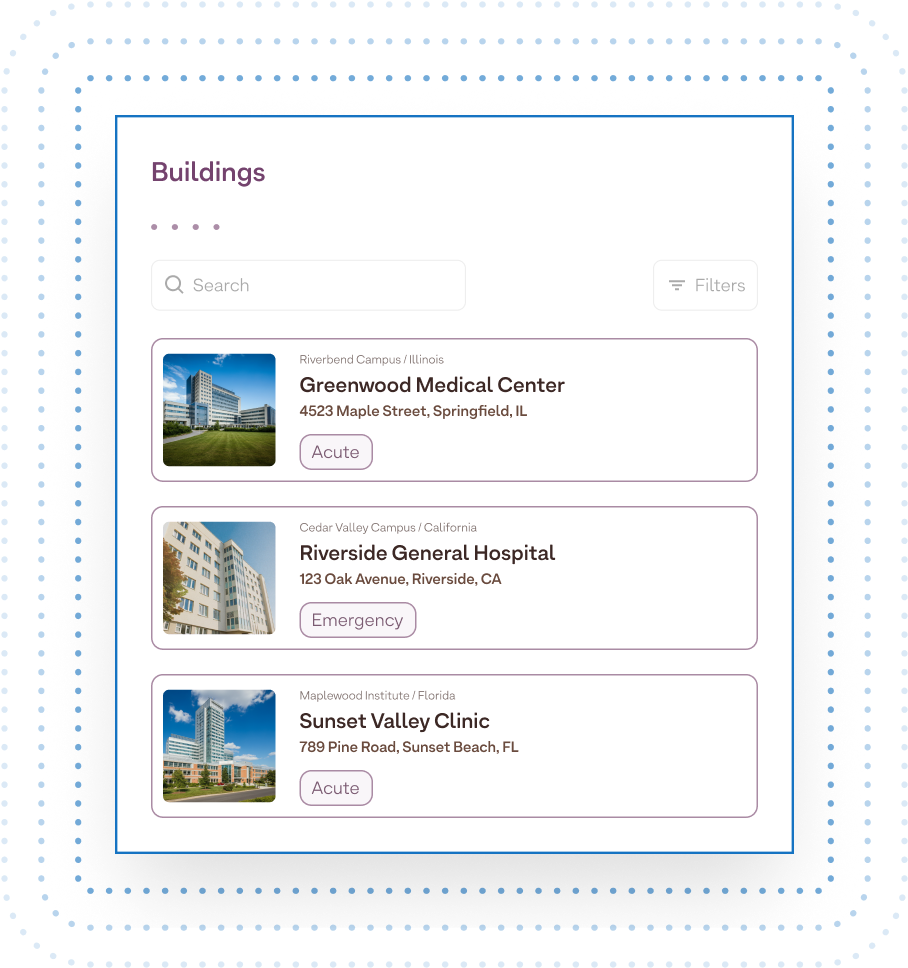
The solution is a structured, building-level system. Each facility should have its own record of assets, vendors, and floor plans. This approach removes confusion and links every compliance check to the physical space it represents.
To build reliable records, focus on:
- Version control: Update drawings and documents in real time.
- Building-level structure: Organize by facility, not just system.
- Integrated directories: Link vendors and assets directly to locations.
Our platform helps address these needs with real-time floor plan updates across multiple formats (PDF, DWG, Revit) and a centralized vendor directory organized by building. Facilities staff gain accurate information at the point of use, not weeks later.
4. Train staff on compliance procedures and responsibilities
Even the best systems fail without well-trained staff. Compliance managers must ensure every employee understands both the standards and their responsibility in meeting them.
To make training effective:
- Tailor content: Adapt by role so each group focuses on what they control.
- Update regularly: Refresh materials when regulations change.
- Test retention: Use short assessments to confirm knowledge, not just attendance.
- Track progress: Document completions to prove audit readiness.
Additionally, training should not be a one-off orientation. Teams need recurring sessions tied to code updates, internal audits, or new equipment. This helps staff connect regulations to daily tasks and reduces the chance of overlooked requirements.
Facility and operations managers should also vary training formats. Some staff benefit from structured classroom-style refreshers, while others retain more through on-site walkthroughs or digital microlearning modules.
A good way to ensure all staff members are carried along is by switching up the training formats. Some employees learn best through structured refreshers, while others benefit from on-site walkthroughs or quick digital modules that fit into their workflow. There’s no one-size-fits-all approach to training; the goal is to ensure that everyone understands their responsibilities in maintaining compliance.
5. Monitor performance, run audits, and address gaps
Compliance isn’t static. Standards evolve, facilities grow, and processes change. Without continuous monitoring, small issues pile up, only to surface during external audits. The best leaders build systems that spot problems early, long before regulators do.
The most reliable way to stay ahead is through internal audits. These reviews show where processes are breaking down, whether it’s missed inspections, outdated floor plans, or incomplete records. When audits happen often, teams can fix issues quickly and stay ready for external reviews.
When setting up monitoring and audit processes, focus on:
- Frequency: Run internal audits often enough to catch issues early.
- Traceability: Connect each finding to the right data, asset, or vendor.
- Follow-up: Document every fix and confirm it’s complete.
But monitoring shouldn’t stop there. Real-time visibility into inspection data, maintenance logs, and vendor activity helps leaders spot trends and recurring gaps, like the same issue appearing across multiple buildings. These patterns highlight deeper problems that need attention, not just quick fixes.
Our platform supports this approach by centralizing inspection histories and linking them to building-level records. This lets teams see exactly where compliance is strong and where recurring problems exist. It also reduces the time spent preparing for external surveys.
Best practices for maintaining compliance in healthcare
- Integrate compliance with capital planning: Build code requirements and inspection steps into renovation and expansion projects so new facilities are audit-ready from day one.
- Use cross-functional reviews: Bring facilities, compliance, and clinical teams together to uncover blind spots and align on corrective actions using shared data.
- Prioritize high-risk areas: Focus tighter monitoring on surgical suites, labs, and emergency zones where lapses have a greater impact.
- Automate escalation paths: Set up automated alerts and workflows so critical issues reach leadership fast and get resolved before audits.
- Keep one source of truth: Use a centralized system like Ruya to link inspections, floor plans, and vendor data by building, ensuring everyone works from the same accurate information.
Maintain healthcare compliance better with Ruya
Maintaining healthcare compliance requires structured inspections, accurate records, trained staff, and proactive monitoring. The process is complex, but the right tools make it manageable, especially when compliance must scale across multiple hospital buildings.
At Ruya, we simplify this challenge by bringing everything together in one place, from mobile inspections and real-time floor plans to building-level vendor directories. By linking compliance data directly to each facility, Ruya helps teams work from accurate information and be ready for audits all year round.
Book a demo today to see how Ruya can help your hospital maintain compliance at all times.

.svg)


